- Vos T et al Lancet. 2016;388(10053):1545–602
- Abbaspour N, Hurrell R, Kelishadi R. Review on iron and its importance for human health. J Res Med Sci. 2014;19(2):164-174.
- Beard JL. Iron Biology in Immune Function, Muscle Metabolism and Neuronal Functioning. J Nutr. 2001:568-580.
- Piñero DJ, Connor JR. Iron in the Brain: An Important Contributor in Normal and Diseased States. Neurosci. 2000;6(6):435-453.
- Radlowski EC Johnson RW Perinatal iron deficiency and neurocognitive development Front Hum Neurosci. 2013; 7: 585.
- Jáuregui-lobera I. Iron deficiency and cognitive functions. Neuropsychiatr Dis Treat. 2014;10:2087-2095.
- Butler J; An overview of chronic heart failure management. Nurs Times. 2012;108(14/15):16-20
- What is Heart Failure? Available at www.heartfailurematters.org/en_GB/Understanding-heart-failure/What-is-heart-failure Last accessed: September 18th 2019
- Bakogiannis, C., et al., Iron deficiency as therapeutic target in heart failure: a translational approach. Heart Fail Rev, 2019.
- Stugiewicz, M., et al., The influence of iron deficiency on the functioning of skeletal muscles: experimental evidence and clinical implications. Eur J Heart Fail, 2016. 18(7): p. 762-73
- Wong CCY, Ng ACC, Kritharides L, Sindone A. Iron deficiency in heart failure: Looking beyond anaemia. Heart Lung Circ 2016; 25: 209-216
- Drozd M, Jankowska EA, Waldemar Banasiak W, Ponikowski P. Iron therapy in patients with heart failure and iron deficiency. Review of iron preparations for practitioners. Am J Cardiovasc Drugs 2017; 17: 183-201
- Ebner N, von Haehling S. Iron deficiency in heart failure: A practical guide. Nutrients 2013; 5: 3730-3739.
- Macdougall IC. Clinical Kidney Journal, Volume 10, Issue suppl_1, 1 December 2017, Pages i1–i2, https://doi.org/10.1093/ckj/sfx08918
- Babitt JL, Lin HY. Mechanisms of anemia in CKD. J Am Soc Nephrol. 2012;23(10):1631-4.
- National Kidney Foundation. K/DOQI Clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Am J Kidney Dis. 2002;39:S1-S266r.
- Ott C, Liebold A, Takses A, Strauch UG, Obermeier F. High prevalence but insufficient treatment of iron-deficiency anemia in patients with inflammatory bowel disease: results of a population-based. Gastroenterol Res Pract. 2012;2012:595970. doi:10.1155/2012/595970.
- https://www.crohnsandcolitis.org.uk/about-inflammatory-bowel-disease, last accessed: 18 September 2019
- Kappelman MD, Rifas–Shiman SL, Kleinman K, et al. The Prevalence and Geographic Distribution of Crohn’s Disease and Ulcerative Colitis in the United States. Clin Gastroenterol Hepatol. 2007;5(12):1424-1429.
- Baumgart DC, Carding SR. Inflammatory bowel disease: cause and immunobiology. Lancet. 2007;369(9573):1627-40. doi:10.1016/S0140-6736(07)60750-8.
- Fadi G Mirza, Rezan Abdul Kadir, Christian Breymann, Ian S Fraser & Ali Taher. Impact and management of iron deficiency and iron deficiency anemia in women’s health
- Percy L, Mansour D, Fraser I. Iron deficiency and iron deficiency anaemia in women. Best Pract Res Clin Obstet Gynaecol. 2017;40:55-67.
- WHO Action framework to advance universal access to safe, effective and quality assured blood products 2020-2023. World Health Organization. at https://www.who.int/news-room/detail/19-02-2020-who-action-framework-to-advanceuniversal-access-to-safe-effective-and-quality-assured-blood-products-2020--2023
- Shander, A. et al. (2020) The Essential Role of Patient Blood Management in a Pandemic- a Call for Action. Anesthesia&Analgesia, doi: 10.1213/ANE.0000000000004844
- Frank, S.M, Oleyar, M.J, Ness, P.M, Tobian, A.A. (2014) Reducing unnecessary preoperative blood orders and costs by implementing an updated institution-specific maximum surgical blood order schedule and a remote electronic blood release system. Anesthesiology, 21(3):501-9
- Leahy, M.F. et al. (2017). Improved outcomes and reduced costs associated with a health-system-wide patient blood management program: a retrospective observational study in four major adult tertiary-care hospitals. Transfusion, 57(6):1347-1358

IRON DEFICIENCY
A GLOBAL LEADER IN IRON DEFICIENCY TREATMENT
CSL Vifor has been a pioneer in the development of iron-based products and has established itself as a global leader in the treatment of iron deficiency.
Our leadership is built on our scientific, regulatory and commercial expertise, resulting in the creation of globally trusted brands including Venofer® and our strategic growth driver Ferinject®. With our iron deficiency and iron deficiency anaemia expertise in heart failure, kidney disease, gastroenterology or inflammatory bowel disease, patient blood management and woman’s health, we help patients affected by these conditions to live better, healthier lives. Iron deficiency is a highly common condition, which is present in up to one third of the global population.
Förtydligande i förhållande till CSL Vifors kommunikation rörande Monofer
Præciseringer i forbindelse med CSL Vifors kommunikation om Monofer
Selvennyksiä liittyen CSL Viforin Monofer viestintään

WHY IS IRON IMPORTANT FOR THE BODY?
Iron is involved in a wide variety of metabolic processes, including oxygen transport, DNA synthesis, and energy production2
In the human body, it is needed for the proper functioning of many systems, including the heart, muscles and red blood cells. It also plays a vital role in the immune system3, the development of the brain4,5 and cognitive function6.
Iron is a fundamental mineral needed to produce hemoglobin, a protein in red blood cells that carries oxygen around the body. Iron deficiency indicates a condition in which iron levels are below the minimal threshold.
If iron levels fall too low and are not treated, the body is unable to produce an adequate amount of hemoglobin and healthy red blood cells, a condition called Iron deficiency anemia, which results in unpleasant symptoms that affect the quality of life.

WHAT ARE THE CONSEQUENCES OF IRON DEFICIENCY?
Iron deficiency worsens with debilitating symptoms such as fatigue, lack of energy and decrease of physical activity.
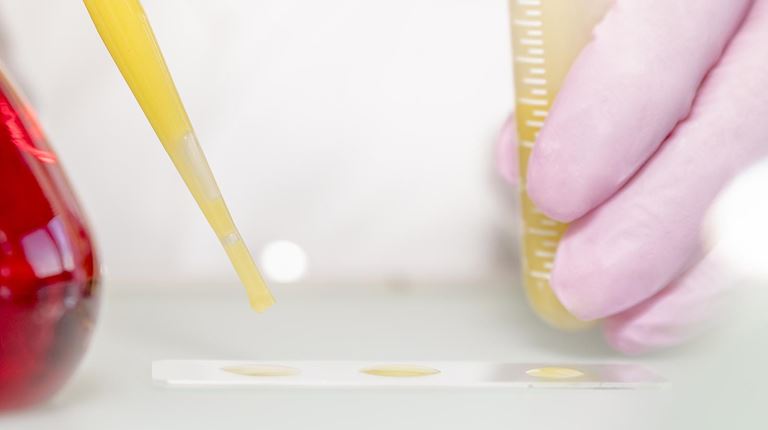
Despite its high occurrence and its potentially serious consequences for many patients, iron deficiency remains an under-diagnosed and under-treated condition Iron levels are routinely assessed through a blood test that shows iron parameters such as serum iron, iron saturation and serum ferritin (a protein that helps to store iron in the body). Healthcare professionals can diagnose iron deficiency based on the interpretation of these parameters.

NEW WHO GUIDELINES ON IRON DEFICIENCY DETECTION
The WHO published new guidelines to help the detection of iron deficiency and iron overload. These guidelines provide global, evidence-informed recommendations on the use of indicators for assessing iron status and application of the use of ferritin concentrations, an indicator of iron storage.
Download the PDF to find out more.
CHRONIC KIDNEY DISEASE
What is chronic kidney disease?
The prevalence of chronic kidney disease (CKD) is relatively high among the adult population, with a prevalence of up to 13%14. Chronic kidney disease is defined as either kidney damage or decreased kidney function for 3 or more months.16
Hypertension, diabetes and heart failure are the main contributing risk factors for developing CKD. The occurrence of CKD is also increasing worldwide as the population ages. Although CKD cannot be reversed, medication is often used to treat associated complications and to slow down further kidney damage. .
Why are patients with CKD at risk for Iron Deficiency?
Iron deficiency in CKD arises from a combination of poor dietary iron intake, impaired absorption of iron by the gut, and greater iron losses, particularly among CKD patients treated with haemodialysis.14,15

INFLAMMATORY BOWEL DISEASE
What is inflammatory bowel disease (IBD)?)?
IBD is an auto-immune condition that affects the gastrointestinal tract and causes inflammation of the gut. The two most common forms of IBD are Crohn’s disease and ulcerative colitis (UC).17 In the UK and USA, around 1 in 250 people have IBD.18,19 The exact etiology of these diseases is unknown and it is thought to be multifactorial, involving smoking, genetics and previous infections.20
Why are people with IBD at risk from Iron Deficiency?
In IBD, the inflammation in the gut leads to both bleeding and reduced iron absorption. For this reason, iron deficiency is frequently associated with IBD.

WOMEN’S HEALTH
Iron deficiency and iron deficiency anaemia are highly widespread among women, particularly those suffering from heavy menstrual bleeding, or who are pregnant, or in the postpartum period.21
Iron deficiency anaemia in pregnancy bears risks for the foetus, such as low birth weight and developmental delays.22 Iron deficiency without anaemia affects up to 33% of menstruating women in Europe.22 Symptoms are often nonspecific, however can include fatigue, irritability, hair loss, poor concentration, palpitations, and dizziness. In severe cases of iron deficiency anaemia, tachycardia, ankle edema, and heart failure may arise.22
PATIENT BLOOD MANAGEMENT
What is Patient Blood Management?
Patient blood management consists of measures designed to improve surgical and medical patient outcomes by optimally managing and preserving patient’s blood.
It has three basic aims: to correct anaemia and iron deficiency, to minimise blood loss and bleeding, and to establish the appropriate use of blood transfusion. Preoperative anaemia is associated with increases in length of stay, surgical complications, mortality and increased rates of transfusions. By treating preoperative anaemia, PBM leads to reduced morbidity, lower transfusion rates and reduced hospital costs, without increasing in-hospital mortality, and even reducing it. PBM should therefore be considered as a strategic approach in times when there is an urgent need to optimise healthcare resources and reduce the pressure on the blood supply. Find out more about PBM on ifpbm.org
What is the effect of PBM on patients, hospitals and health care systems?
Large observational studies on PBM including anaemia management have demonstrated PBM effectiveness in improving patient outcomes.
Moreover, studies around the world have shown that the implementation of PBM programmes can contribute to lower hospital costs and benefit national healthcare budgets.
One real-world-study more than 600,000 patients in Western Australia confirmed these findings and demonstrated a 41% reduction of allogeneic blood transfusions with cost savings of more than 80 million dollars.26
Are you a healthcare professional and you want to know more about the benefits of PBM? Visit the dedicated website below!

